Note: Today is an opinion piece on options for prostate cancer. It is MUCH more opinion based than some other entries on the blog – just a note. I still think the topic is valuable and writing these helps me to organize my thinking.
Today, we’ll look at options for prostate cancer and talk about the number of options available and then look a bit closer at the radiation side of “standard of care” treatment options.
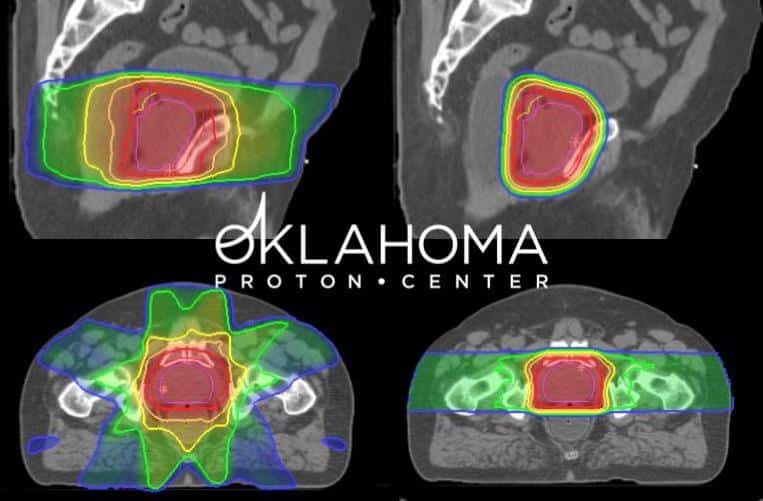
At the Oklahoma Proton Center, we end seeing and caring for a large number of men diagnosed with prostate cancer. Generally, most of the men we see have been on the internet and looked at available options or they’ve seen the recent lawsuit against Aetna for $25.5M for denying proton therapy or they’ve had a friend or acquaintance who has been treated with proton therapy – point being, they have taken a more active role in their care and present to our center for evaluation.
Difficulty of Choosing a Prostate Cancer Treatment Plan
Nearly all of our proton therapy patients are advocates for themselves. You generally don’t just end up at a Proton facility without the patient taking initiative.
More recently, I’ve come to realize just how confusing the current landscape is for some patients – especially those with prostate cancer.
Options for the care of prostate cancer range from Active surveillance (a fancy name for observation and following of the disease) to invasive procedures like surgery or robotic prostatectomy or brachytherapy options. In some areas, cyrotherapy or HIFU is discussed as an option for up front diagnosis. So even there we have listed off a good handful of options that are available to you.
Typically, I think the NCCN Guidelines are really very well done and do represent the “standard of care”. For prostate cancer, they are a mess in my opinion.
Now lets look at the mess that is the “standard of care” for external beam therapy. This includes external traditional radiation, IMRT, SBRT and proton therapy. The NCCN guidelines simply group them all together. The NCCN guidelines literally list 16 dose options for low risk and favorable intermediate risk patients. They range from a max of 45 days of treatment to 5. I’d show the table here but for some crazy reason, it really does come with a disclaimer that it is for my personal use only and I cannot distribute the “standand of care” table – how that makes sense – I have no idea – but I’ll respect the crazy idea and not reproduce it here – but trust me – at least 16 dose options are listed as standard.
So I guess the question is that – does this represent a flaw in the NCCN format or does it represent a larger flaw in our larger medical of how we have treated prostate cancer?
It is probably more of the latter. The panel for this guideline is made of 30 individuals and as they try to come together and concisely document current practice patterns. The result of that discussion is what is then represented. In my opinion – a mess.
Prostate Cancer Standard of Care: A Physician’s Opinion
To me, in prostate cancer, we’ve entered the politically correct world of whatever you do, it’s all about the same.
From a scientist / technical viewpoint – I do not believe 20 different treatment approaches for the treatment of prostate cancer are equivalent. I feel strongly there are better options and there are worse options.
The current trend of “non-inferiority” trials further muddles the “standard of care” landscape. It’s important to understand how “non-inferiority” trials are done. First off, they make some large scale assumptions – like this compared treatment will be no worse than 5% worse than our current standard (one I was reading the other day was at 7.5%). Let’s think about that – let’s say that you have a treatment that produces at 94% cure rate. Your saying the trial – mathematically – will show the new treatment is Not Inferior so long as the cure rate is 89% or higher. Think about it another way – that’s a doubling of the failure rate that is deemed equivalent.
To me, it leads us to a place were the NCCN Guidelines actually still list 72 Gy at 2 Gy per fraction as a standard of care option – even for intermediate and high risk disease. MD Anderson ran a great trial back in the 1990’s showing higher doses were simply better. Higher dose became the standard of care, until recently when all these alternate fractionation schedules gained mainstream acceptance.
Long term results of the randomized MD Anderson trial showing benefit of higher doses was published in 2008. 78 Gy obtained 78% disease free survival. 70 Gy obtained 59% disease free survival. Nearly a 20% improvement – cutting the failure rate in half.
I guess the NCCN panel thought they were clever in moving the low end above the clearly inferior 70 Gy standard that was PROVEN to be less effective. And then I guess the argument would be that there is no data showing specifically that 72 Gy is not as effective as 78 Gy, or maybe for some patients maybe you can go lower – I wasn’t in the room. But to me, high dose is the standard. We should move there and simplify.
We should be celebrating the best data and striving to improve upon those results. Not get “close enough” and call that an equivalent new standard.
As physicians, I think we should be helping to define and standardize the treatment of cancer. We are able to do well using a variety of approaches, but they are not all equivalent.
Prostate Cancer Treatment Plan: A Physician’s Recommendations
So I guess I need to step up and make some recommendations. So here are my recommendations – ALL OPINION – Remember – Guidelines say some 20+ options are all pretty much the same:
I’d eliminate lower doses of IMRT – <76 Gy. I’d work to pick EITHER 60 Gy / 20 fractions or 70 Gy / 28 fractions – (personally, we’ve picked 70 Gy / 28 fractions – there is very little data comparing these two head to head). So I’ve eliminated the low dose standard of care options. I think they are too far behind the scenes of today’s options.
So below are my thoughts on various treatment options I’d consider – and I do think I’d probably really have any of these – based on location / income / savings – here is my current thinking:
Proton therapy – traditional treatment at 1.8 – 2 to 7800 – 7920 cGy(RBE) is really good established treatment – fiducial based. Longest data to these doses with a track record back into the 90s – first external treatments to these dose – well before IMRT with a good long-term history and great long-term toxicity data. Straightforward / robust plans. Overall, I believe the simple fact that less radiation given to the bodies normal tissues will be proven to be better in the long-term. (I’m probably biased, but the data is consistent and long-term).
Implant – great treatment but less consistent – at super high volume center – maybe as good or better than anything with good patient selection. (for a number of reasons, brachytherapy is on the decline and being replaced by the logistically easier external options – that is probably another blog entry or two at some point).
Cyberknife treatment to 3500-4000 cGy in 5 fractions – likely daily or weekly – fiducial based. Some very strong current data showing excellent results in a quick treatment course. (Some excellent results – I believe the old simple saying of “there is no free lunch” – If you look at the Proton trial comparing 44 to 5, side effects all tended to be a bit worse in the short course treatment arm. As of today, I think this is the trade off – quicker, bit less expensive – bit more acute and long term side effect risks).
Next tier:
SBRT – can probably be as good as Cyberknife treatment. I do think you gain some consistency within the Cyberknife framework and the tracking is different and the fiducial placement is more consistent within the Cyberknife environment. SBRT can be very high quality but for the same reason I bumped down Implants a tier, I’ve moved this here.
IMRT is good treatment – high volume center / high dose – either conebeam or fiducials need to be part of the treatment. I don’t believe that nadir data is as good and I don’t think the data holds up as well as other approaches when measured using a very strict PSA criteria. Toxicity wise, I believe it still struggles to produce a very low toxicity profile – that’s why you see low dose IMRT listed in the NCCN guidelines. That is a problem that simply stated, hasn’t happened in the proton literature. With protons you can deliver ~80. With IMRT that carries more risk. It’s still good treatment and does very well with control, but as of today, I think traditional fraction IMRT radiation is in the process of being replaced by better options.
Prostate Cancer Treatment Discussion
I realize that many very well educated treating physicians might have very strong disagreements with the above tiers. Many would argue that results are good enough using any approaches and that, in particular, there is no reason or data to support proton therapy in this cancer.
But I didn’t think it was fair to write this entry and not give my opinion as of today. I try to constantly read and keep up with the literature – probably much of what we think today will be wrong in 5 years, but we need to simplify information < that I’m sure of.
Why do I think the above options are better? I think the three places where you see a PSA bounce (ie the PSA falls and then temporarily rises) are with implants, protons, and SBRT approaches. Traditional IMRT doesn’t cause a bounce as often in my experience. I don’t think the doses are consistently as high and therefore I don’t think its “the best available”. The top three options have a PSA bounce and have produced low toxicity profiles in high volume institutions.
My guess on the future of Prostate Cancer Treatment with Radiation:
Based on my review of the literature, I think we have two current paths gaining momentum, that I think, offer advantages over traditional IMRT – Protons and SBRT. HDR and implants have very good data, but as logistics improve with less invasive approaches, the logistical benefit of an implant decreases. My guess is, over the next 10 years, these two paths forward will come together and the very best outcomes can potentially be with less treatment fraction programs using Proton Therapy instead of traditional x-rays.
In the meantime, I think we would serve patients better by working to simplify recommendations for the treatment of prostate cancer and move away from our current perspective where it seems that really, anything is pretty good and pretty good is good enough.
We have many good treatment options and access vs. the very best treatment is always a factor, but we should not confuse easy patient access for treatment and answering the question of “which treatments are truly the best”? To me, in prostate cancer we’ve confused the two a bit too often and the result is not good for advancing treatments forward for the current and future generation of prostate cancer patients.
